Understanding Osteoarthritis Joint Pain: What Causes It, What Are the Symptoms, and What Can Help
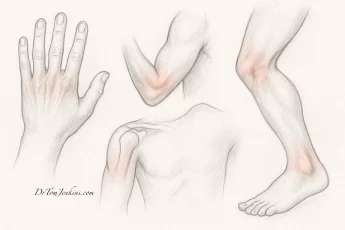
Osteoarthritis (OA) is one of the most common causes of joint pain and stiffness, especially in people over 50. It can affect any joint but is most often found in the knees, hips, hands, and spine. In Gloucestershire and the Cotswolds, many people live with the daily discomfort of osteoarthritis—but there are effective ways to manage the symptoms and reduce pain.
Osteoarthritis doesn’t just cause aches—it can also lead to a significant loss of mobility, reduced independence, and increasing reliance on painkillers. It may stop you from enjoying exercise, playing sport, or even joining friends for a walk or round of golf. As it becomes more severe, it can begin to limit everyday functioning—such as how far you can walk, managing stairs, or even simple daily tasks like dressing, cooking, or getting out of a chair can become a real challenge. These physical restrictions can be frustrating and isolating—but the good news is that this doesn’t have to be your new normal. With the right care, support, and understanding, there are often ways to reduce your symptoms and restore your confidence and freedom.
Symptoms of Osteoarthritis: What to Look Out For
If you’re wondering whether your joint pain could be caused by osteoarthritis, here are the typical signs to look out for:
Joint pain – Often described as a deep, aching pain that worsens with activity and improves with rest.
Stiffness – Especially in the morning or after inactivity. Morning stiffness typically lasts less than 30 minutes in OA.
Reduced mobility – Difficulty with bending, squatting, twisting, or reaching.
Grinding, clicking or creaking – Known as crepitus, this can be felt or heard when moving the joint.
Swelling – Particularly in weight-bearing joints like knees and hips, or in smaller joints like fingers during flare-ups.
Joint instability or giving way – Especially in the knee, which can make you feel less confident during activity.
Bone spurs – Small, bony lumps may form around affected joints, especially in the hands.
For more detail, visit Versus Arthritis – Osteoarthritis.
Where Does Osteoarthritis Pain Come From?
It’s a common myth that osteoarthritis pain comes from “bone-on-bone” contact. In fact, the surfaces of your bones and cartilage don’t have nerve endings — so they can’t directly feel pain. Instead, most of the discomfort comes from other tissues in and around the joint.
The two main contributors to pain in osteoarthritis are joint instability and biochemical inflammation, followed by other structural issues that can add to the problem.
1. Joint instability and mechanical strain
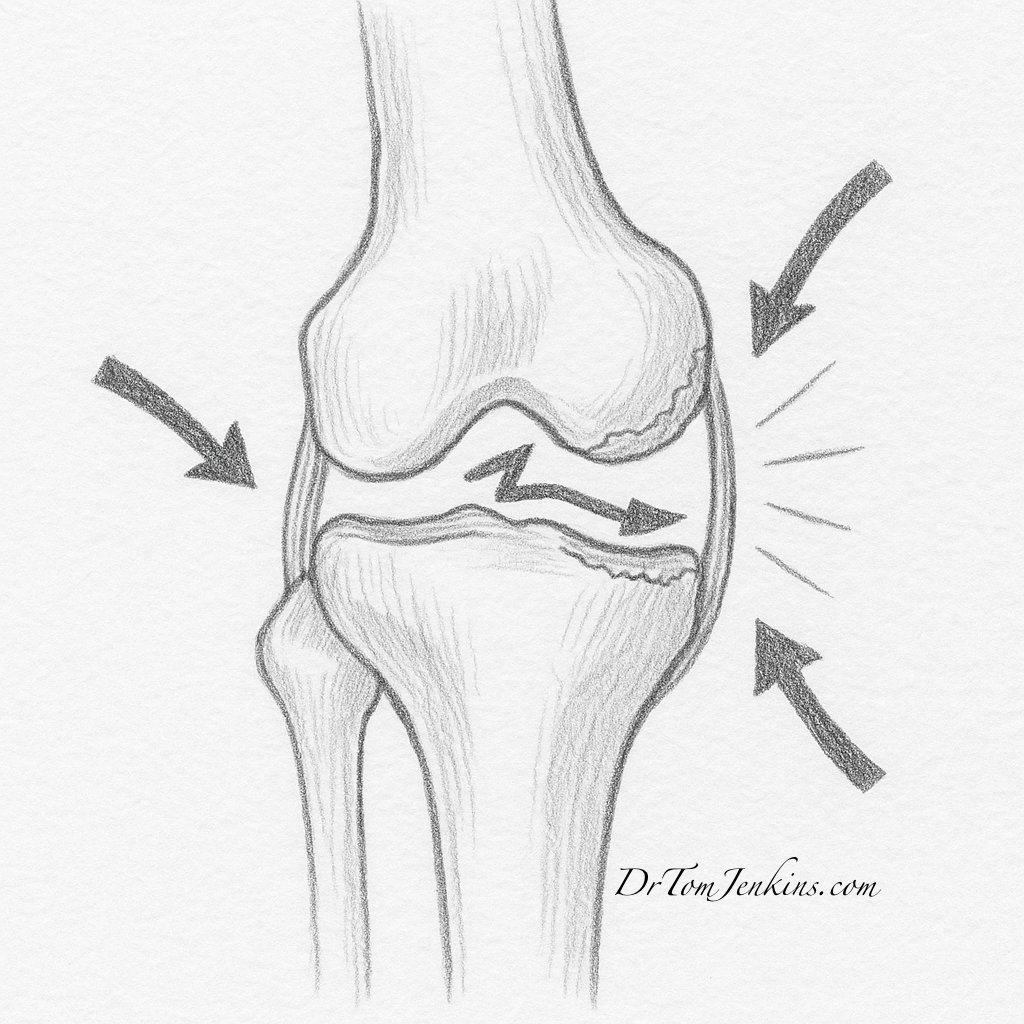
As cartilage wears away and muscles around the joint weaken, the joint can become unstable. This leads to abnormal movement patterns and mechanical strain on the surrounding soft tissues — including the joint capsule, ligaments, and tendons — all of which contain many nerve endings.
Why physical therapy can help:
Strengthening small stabilising muscles — like vastus medialis (in the knee) or gluteus medius (in the hip) — improves control and support around the joint. When the joint moves more smoothly and with better alignment, these tissues are less likely to become irritated. This leads to reduced pain, better function, and less reliance on medication.
2. Biochemical inflammation of sensitive joint tissues
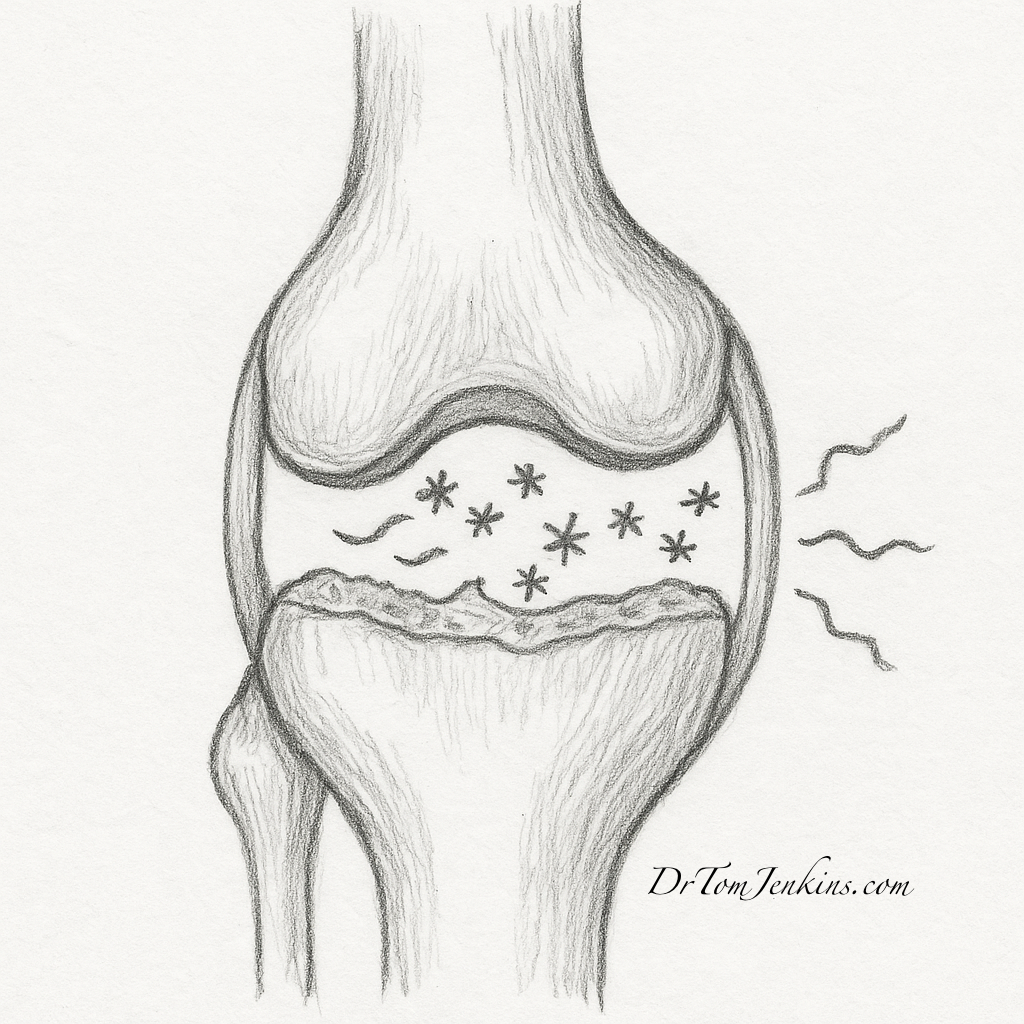
The inside of the joint is lined with a membrane called the synovium. In osteoarthritis, this lining can become inflamed (synovitis), releasing chemical signals that irritate the nerves in the joint capsule. This creates a dull, aching pain — often felt even at rest or overnight.
How steroid injections help:
Corticosteroid injections reduce this inflammation by calming the chemical messengers that trigger pain and swelling. This can provide rapid relief from inflammation-related symptoms, especially during a flare-up.
3. Other contributors to osteoarthritis pain
- Bone marrow lesions and microfractures: Small areas of swelling and stress in the bone beneath the joint surface, often very painful but invisible on X-rays.
- Osteophytes (bone spurs): Bony outgrowths that can press on nerves or soft tissues, causing sharp, localised pain.
- Chronic synovitis: Long-lasting inflammation of the joint lining can cause persistent swelling, tenderness, and stiffness.
- Muscle imbalance: Weakness or poor movement patterns lead to increased joint strain and reinforce a cycle of pain and inactivity.
4. What about PRP and hyaluronic acid injections?
Platelet-Rich Plasma (PRP):
PRP is made from your own blood, spun in a centrifuge to concentrate growth factors. These may help calm inflammation, reduce pain signalling, and support natural tissue healing. It’s most effective in early to moderate osteoarthritis.
Hyaluronic acid (HA) injections:
HA is a gel-like lubricant found in healthy joint fluid. In osteoarthritis, this fluid becomes thinner. HA injections help restore cushioning and improve joint movement — particularly in the knee.
Both of these are available privately in the UK but not generally under the NHS.
Osteoarthritis Treatments: What Else Can Help?
In addition to rehab and injections, these additional measures can also make a big difference:
Weight management — not just for weight-bearing joints
It’s well known that losing weight reduces strain on joints like your knees and hips — but that’s only part of the story. Studies show that weight loss can also improve symptoms in joints that don’t bear weight, such as the hands. This is because fat tissue releases inflammatory chemicals (like cytokines and adipokines) that circulate in the bloodstream and worsen joint inflammation. By reducing body fat, you lower these systemic inflammatory signals, which may ease pain across multiple joints — not just those carrying your weight.
So even small, sustainable changes in weight can improve your symptoms more broadly than most people expect.
Footwear and orthotics
Wearing well-cushioned shoes and using insoles or braces can help redistribute pressure and improve comfort during daily activity.
Activity modification and pacing
Learning to balance movement with rest — and choosing joint-friendly activities — can help you stay active without aggravating symptoms.
Osteoarthritis FAQs: Your Questions Answered
Will exercise make osteoarthritis worse?
No — in fact, regular movement is one of the best ways to manage symptoms. According to Versus Arthritis, strengthening the muscles around the joint helps reduce pain and improve function. Avoiding movement often leads to further stiffness and weakness.
Can I still walk, run, or play sport with osteoarthritis?
Yes — especially with guidance. Walking, swimming, cycling, Pilates, and resistance training are all helpful. You may need to modify higher-impact activities, but many people continue to enjoy sport with the right support.
Do I need a joint injection?
Not necessarily — but injections can be very effective when symptoms flare or conservative treatments haven’t worked. Where needed, I use ultrasound-guided techniques to ensure precise, comfortable delivery.
Is osteoarthritis just part of getting older?
While OA is more common with age, it doesn’t always lead to disabling pain. Many people stay active for decades with the right support and early treatment.
My Approach to Helping People with Osteoarthritis Pain
Osteoarthritis doesn’t just affect joints — it affects your confidence, your independence, and your ability to enjoy life. You might avoid walks, decline sport with friends, or struggle with basic tasks. But that doesn’t have to be your reality.
I believe that pain and limitation are not things you simply have to accept with age. My approach is about helping you understand what’s causing your symptoms, and then working together to reduce pain, improve movement, and restore your confidence — whether through tailored rehab, joint injections, or other options that work for you.
Get in Touch for Personalised Help in Gloucestershire and the Cotswolds
If you’re based in Gloucestershire or the Cotswolds and are struggling with joint pain, stiffness, or reduced mobility due to osteoarthritis, I’d be happy to help. I offer private consultations, joint injections, and rehabilitation planning , often working with local therapists, coordinating imaging and helping you understand your options.
To find out more or to book an appointment, visit www.drtomjenkins.com or contact me directly. You don’t have to accept pain and limitation as your future — there are effective treatments, and I’m here to help you explore them.