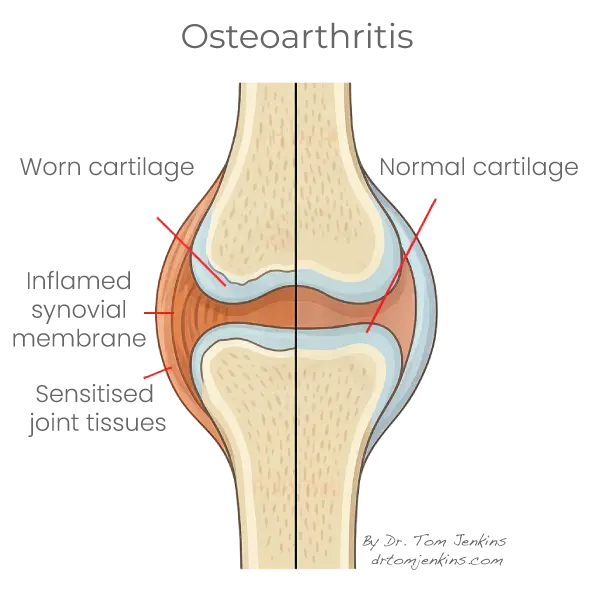
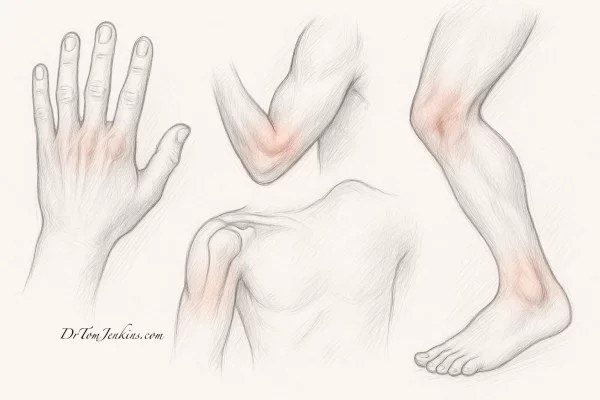
Osteoarthritis is the most common form of arthritis and a leading cause of joint pain and stiffness, particularly in older adults. It can affect any joint, but is especially common in the knees, hips, hands, feet, spine and shoulders.
Osteoarthritis develops when the cartilage that cushions the ends of bones gradually wears away. As the joint loses its smooth surface, bone may rub against bone, leading to inflammation, swelling, stiffness and pain. The surrounding tissues — including the synovial lining, joint capsule, ligaments and small postural muscles — can become sensitised and contribute to ongoing discomfort and reduced mobility.