Many people come to clinic describing an ache or tenderness on the outside of the upper thigh that makes it uncomfortable to lie on that side in bed, walk long distances, or return to sport. For some, it’s a low-level niggle. But for others, hip pain can become deeply distressing — stopping them from sleeping, limiting exercise, and even making everyday activities like walking or climbing stairs painful.
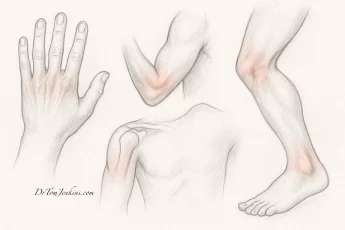
In cases like this, what most people think of as “hip pain” isn’t coming from the hip joint itself. Instead, it’s often caused by the soft tissues that sit over the outer upper thigh — particularly near the greater trochanter, a bony prominence on the side of the hip.
This region is the meeting point of several important structures: gluteal tendons, bursae, fascia, and the iliotibial band. Because of this anatomical overlap, outer hip pain is rarely caused by just one issue. In fact, what seems like a simple problem is often more complex and nuanced, with several contributing factors. A thorough clinical assessment is essential to correctly identify what’s causing the pain — and to ensure that treatment targets the right structures.
What is Greater Trochanteric Pain Syndrome (GTPS)?
GTPS is a broad term used to describe pain and dysfunction in the soft tissues around the greater trochanter. It typically includes:
- Gluteal tendinopathy — often involving the gluteus medius and minimus tendons
- Trochanteric bursitis — inflammation of the fluid-filled sacs (bursae) that reduce friction
- Iliotibial band irritation — compression or tension in the fibrous band running down the outer thigh
GTPS is particularly common in people over 40, especially women, and in runners or walkers. It’s often caused by a combination of overload and underload — too much repetitive strain on the area, combined with muscle weakness or poor pelvic stability.
It may also develop alongside lower back pain or sacroiliac joint dysfunction, which can alter posture and gait, placing extra strain on the tissues around the hip.
How Outer Hip Pain Affects Your Life
Pain over the side of the hip can be surprisingly disruptive.
Many people find they can’t lie on the painful side in bed — and even rolling over can disturb sleep. If you’re active, you may find that running, cycling or long walks bring on discomfort. Even walking up stairs or standing still for too long can set things off.
This type of hip pain at night, or hip pain when walking, often leads people to reduce or stop their usual activities — which in turn weakens the supporting muscles further, making the problem worse.
Over time, it can affect sleep, movement, and confidence. But the good news is that once the correct structures are identified, targeted treatment can be highly effective.
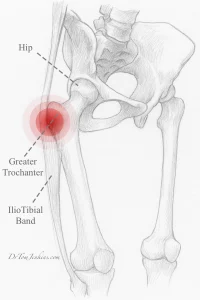
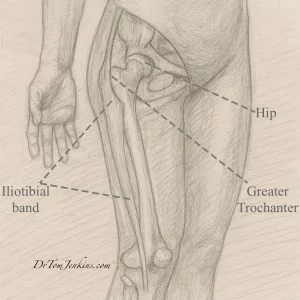
Understanding the Iliotibial Band (ITB)
The iliotibial band (ITB) is a thick band of fibrous tissue that runs from the pelvis, down the outside of the thigh, to just below the knee. It helps stabilise the hip and knee — particularly during walking and running.
The ITB often contributes to outer hip pain through tension, compression or friction over the greater trochanter, or due to mechanical overload. Importantly, pain can occur at different points along the band, not just the hip — including the mid-thigh and outer knee, where it may present as iliotibial band friction syndrome (ITBFS).
Stretching the ITB: What Patients Need to Know
Stretching the ITB is often recommended — but success depends on understanding a few key points:
The ITB is extremely strong and fibrous — it takes time to stretch, often 3–6 months of daily effort.
Not all stretches suit everyone — different postures and body types require tailored approaches.
Effective stretching often requires guidance from a physical therapist, to ensure it’s targeting the right area without aggravating symptoms.
It’s easy to lose confidence if the pain doesn’t improve right away — but with a personalised programme, consistency pays off. And when done alongside strength work for the gluteal muscles and movement retraining, stretching becomes a crucial part of long-term improvement.
The Role of Injections
For patients with severe pain or difficulty progressing in rehab, an ultrasound-guided steroid injection can help reduce inflammation and provide rapid relief. In selected cases, hyaluronic acid or PRP (platelet-rich plasma) injections may be offered as well.
However, injections are not a standalone cure. They are best seen as a way to create a window of reduced pain so you can fully engage in your rehabilitation programme.
Injections provide quick relief — but stretching and strengthening give lasting relief.
Diagnosing Outer Hip Pain Thoroughly
Because so many different — and often overlapping — structures can cause similar symptoms, a careful clinical assessment is essential. In my clinic, I take time to:
- Understand the history of your pain
- Examine posture, gait and movement patterns
- Test strength, tension, and compression of specific muscles and tendons
- Use diagnostic ultrasound to assess the gluteal tendons, ITB, and bursa
- Rule out referred pain from the spine or sacroiliac joints
A proper diagnosis allows us to guide your rehab and, where necessary, target injections precisely for the best result.
Getting the Right Help
If you are struggling with persistent hip or outer thigh pain, I offer private musculoskeletal consultations from my clinic in Gloucestershire.
We provide:
- Thorough clinical assessment and diagnosis
- Rehab planning and referral to trusted physiotherapists
- Ultrasound-guided injections including steroid, hyaluronic acid, and PRP
You can book an appointment online or contact me directly at contact@drtomjenkins.com.
Further Reading and Resources